
Federal government spending big on healthcare plans that aren’t being used
A new report raises concerns about taxpayer waste in federal healthcare programs, as studies show billions of dollars in subsidies and benefits may not be reaching patients, and seniors face the steepest Medicare premium hikes in nearly a decade.
The Wall Street Journal warned that “ObamaCare really is a gift that keeps on giving – for insurers.”
The editorial board cited new findings from the Paragon Institute showing the number of Affordable Care Act enrollees who filed no medical claims tripled from 3.5 million in 2021 to 11.7 million in 2024.
“More than a third of all enrollees generated no medical claims last year,” The Journal wrote, adding that “tens of billions of dollars in subsidies for these 11.7 million enrollees went to insurers and middlemen without funding a single medical service.”
The Journal noted that “insurance brokers have been fudging incomes of people in order to enroll them in government-subsidized plans for which they aren’t eligible, often without their knowledge.” The editorial also said the Biden administration “facilitated such fraud by easing income verification and eligibility checks.”
If “phantom patients” exist in Obamacare, watchdogs are asking whether the same problem could exist in Medicare Advantage, a much larger program that covers 32 million seniors.
Medicare Advantage will pay out $86 billion in 2025 for supplemental benefits, including dental and vision. However, the Medicare Payment Advisory Commission (MedPAC) concluded this summer that “little is known about the extent to which MA enrollees use the many supplemental benefits available to them,” according to MarketWatch.
Despite being required since 2012 to collect encounter data, CMS did not accept dental data until 2024. MedPAC said this makes utilization data incomplete and unreliable.
CMS Administrator Dr. Mehmet Oz told the U.S. Senate earlier this year that he’d rather cut waste, fraud, and abuse in Medicare Advantage spending than cut Medicaid.
“The former sounds like a more rational way to do that,” he said during his Senate confirmation hearing.
Republicans say CMS or the Government Accountability Office already has the power to review how many Medicare Advantage enrollees file zero claims in a year and to verify whether supplemental benefits are being used.
Meanwhile, seniors are facing higher Medicare costs.
The standard Medicare Part B premium is projected to rise from $185 per month in 2025 to $206.50 in 2026. That is an 11.6% increase, the largest in nearly a decade. Prescription drug premiums under Part D will likely climb by about 6%, while the annual out-of-pocket cap for drugs will rise from $2,000 to $2,100.
Latest News Stories

Board Confronts Animal Services Crowding, Explores Future Facility Options
Will County Board Members Demand Transparency in Cannabis Tax Fund Allocation

Homer Glenn Residents Push Back on 143rd Street Widening as Officials Signal “Tentative Agreement”
Will County Forges 2026 Federal Agenda Amid D.C. Policy Shifts, ‘Big Beautiful Bill’ Impacts
Health Department Seeks $1 Million Levy Increase to Prevent “Weakened System”
County Rolls Out New “OneMeeting” Software to Improve Public Access

Meeting Summary and Briefs: Will County Board Finance Committee for August 5, 2025
Will County PZC Approves Rezoning for Truck Repair Facility on Manhattan Road Amid Resident Concerns
Key Stretch of Bell Road on Track for Thanksgiving Reopening, Committee Approves Additional Funds
Will County Leglislative Committee Opposes Federal Push for Heavier, Longer Trucks
Will County Reports Progress in Opioid Fight, Highlights New FDA Labeling Rules
In-House Staff Completes Major Renovations at Will County Adult Detention Facility
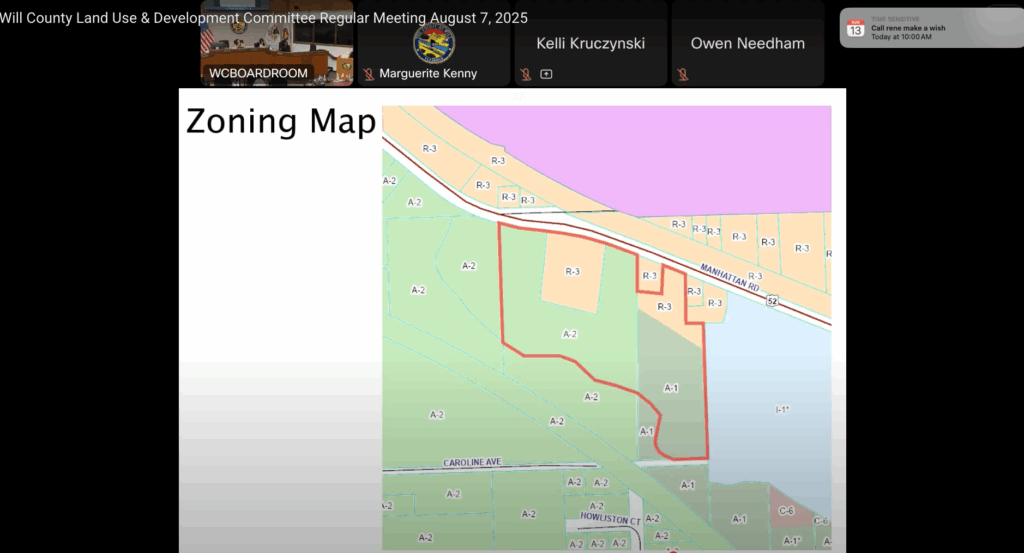
Will County Advances Truck Repair Facility Plan on Manhattan Road Despite Resident Objections

PZC Grants Variance for Oversized Garage in Joliet Township, Reversing Staff Recommendation
