Federal government spending big on healthcare plans that aren’t being used
A new report raises concerns about taxpayer waste in federal healthcare programs, as studies show billions of dollars in subsidies and benefits may not be reaching patients, and seniors face the steepest Medicare premium hikes in nearly a decade.
The Wall Street Journal warned that “ObamaCare really is a gift that keeps on giving – for insurers.”
The editorial board cited new findings from the Paragon Institute showing the number of Affordable Care Act enrollees who filed no medical claims tripled from 3.5 million in 2021 to 11.7 million in 2024.
“More than a third of all enrollees generated no medical claims last year,” The Journal wrote, adding that “tens of billions of dollars in subsidies for these 11.7 million enrollees went to insurers and middlemen without funding a single medical service.”
The Journal noted that “insurance brokers have been fudging incomes of people in order to enroll them in government-subsidized plans for which they aren’t eligible, often without their knowledge.” The editorial also said the Biden administration “facilitated such fraud by easing income verification and eligibility checks.”
If “phantom patients” exist in Obamacare, watchdogs are asking whether the same problem could exist in Medicare Advantage, a much larger program that covers 32 million seniors.
Medicare Advantage will pay out $86 billion in 2025 for supplemental benefits, including dental and vision. However, the Medicare Payment Advisory Commission (MedPAC) concluded this summer that “little is known about the extent to which MA enrollees use the many supplemental benefits available to them,” according to MarketWatch.
Despite being required since 2012 to collect encounter data, CMS did not accept dental data until 2024. MedPAC said this makes utilization data incomplete and unreliable.
CMS Administrator Dr. Mehmet Oz told the U.S. Senate earlier this year that he’d rather cut waste, fraud, and abuse in Medicare Advantage spending than cut Medicaid.
“The former sounds like a more rational way to do that,” he said during his Senate confirmation hearing.
Republicans say CMS or the Government Accountability Office already has the power to review how many Medicare Advantage enrollees file zero claims in a year and to verify whether supplemental benefits are being used.
Meanwhile, seniors are facing higher Medicare costs.
The standard Medicare Part B premium is projected to rise from $185 per month in 2025 to $206.50 in 2026. That is an 11.6% increase, the largest in nearly a decade. Prescription drug premiums under Part D will likely climb by about 6%, while the annual out-of-pocket cap for drugs will rise from $2,000 to $2,100.
Latest News Stories
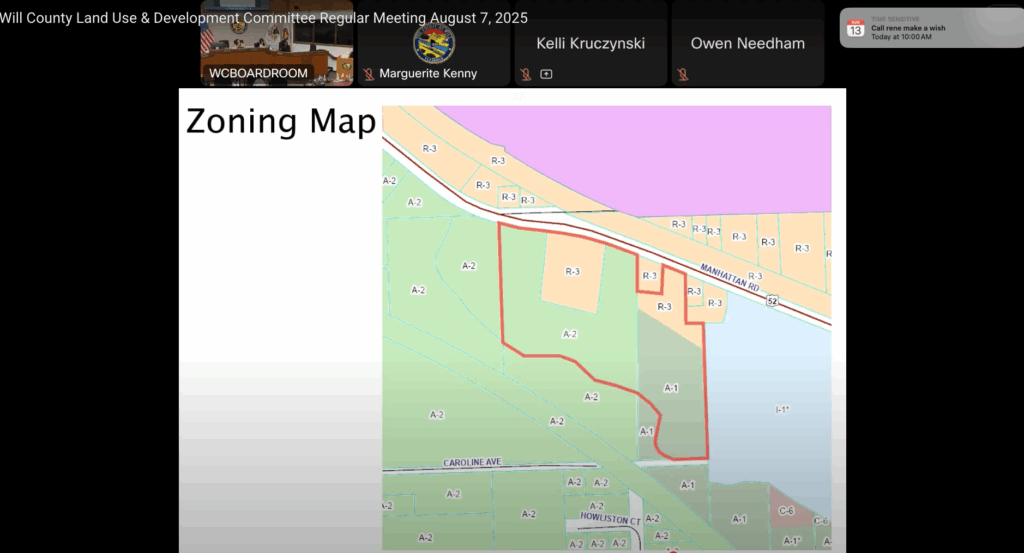
Will County Advances Truck Repair Facility Plan on Manhattan Road Despite Resident Objections

PZC Grants Variance for Oversized Garage in Joliet Township, Reversing Staff Recommendation

Will County Public Works Committee Approves Over $1.1 Million in New Agreements for 80th Avenue Project

Meeting Summary and Briefs: Will County Board Legislative Committee for August 5, 2025

Meeting Summary and Briefs: Will County Board Capital Improvements & IT Committee for August 5, 2025

Meeting Summary and Briefs: Will County Land Use & Development Committee for August 7, 2025

Meeting Summary and Briefs: Will County Planning and Zoning Commission for August 5, 2025

Meeting Summary and Briefs: Will County Public Works & Transportation Committee for August 5, 2025

Beecher Fire District Promotes Three to Lieutenant/Paramedic

Fire Board Approves $13,895 Landscaping Contract for Station

Meeting Summary and Briefs: Beecher Fire Protection District Board of Trustees for June 26, 2025

Meeting Summary: Peotone School District 207-U for July 21, 2025